Orthobiologic Platform
Orthobiologics
The term Orthobiologics refers broadly to any treatment type aimed at promoting or stimulating a healing response in tissues. Most advances in surgery over the last several decades have focused on improving the mechanical strength of surgical repairs and reconstructions.
For most procedures today, reliable and effective repair can be obtained with the strength necessary to allow for early rehabilitation and motion. Early skilled therapy greatly improves the outcomes associated with surgery.
The new horizon in improving outcomes for our patients is to improve the quality and possibly the speed of healing tissue through biologic interventions. Based on the type of tissue being treated and what the underlying problem initially was a variety of different orthobiologic treatments can be used.
The Orthobiologic field is new and still evolving. Large scale clinical research and experimental trials and studies are still being conducted and will ultimately guide the use of these treatments in the future. For now, all of the products discussed below and those in clinical use at the Mammoth Orthopedic Institute have shown good safety profiles, and compelling benefits for our patients. Unfortunately, in many cases, because large scale studies are lacking, these procedures are not covered by health insurance plans. In those cases, we have worked to make our pricing fair and competitive when compared to other centers.
Orthobiologics may be used alone or in conjunction with a surgery or procedure. Ultimately, the decision to undergo one of these treatments should be made in conjunction with your surgeon as part of a larger treatment plan. If you are interested in these treatments and would like more information but are not immediately in the area please contact us for a remote consultation.
Our current platform of treatment options is discussed below:
Platelet Rich Plasma (PRP)
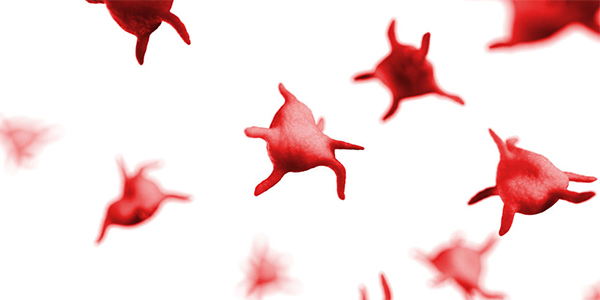
Healing after an injury involves a well-orchestrated and complex series of events where proteins in the blood act as messengers to regulate the entire process. Many proteins involved in the healing process are derived from small cell fragments in the blood called platelets. Platelets are small, colorless, cell fragments present in the blood. They are formed in the bone marrow and are freely passing through the bloodstream in a resting state.
However, when an injury occurs, the platelets become activated and start to gather at the injury site to release beneficial proteins called growth factors. This is the beginning of the healing process. For many years, blood components derived from the patient and then delivered to the site of injury have created growing interest for use in orthopedic procedures. New research and technology has expanded the application of this therapy for use in orthopedic procedures.
What is it?
Platelet Rich Plasma is a concentration of platelets and growth factors created from a small amount of your own blood. Increased levels of growth factors have the potential to improve signaling and recruitment of cells. This concentrated portion of the blood is often referred to as platelet-rich plasma (PRP).
How is it done?
A nurse starts an IV (a small tube placed in a vein) and a small amount of blood is drawn into a syringe. This sample then goes through a rapid spinning process that separates and concentrates the platelets and other beneficial growth factors from the blood. This concentrated portion is then injected into the painful joint or tissue. The entire PRP process is usually done in less than 30 minutes.
What are the risks?
Because PRP uses your body’s own natural properties to treat your injury side effects are very uncommon. There can be an increase in pain and swelling 48-72 hours after the injection and pain immediately after the injection; however, part of this is the mechanism of the PRP working naturally.
For more information about PRP, please proceed to our dedicated page here
Amnion
Amniotic-derived tissues contain regenerative qualities and growth factors that maintain the natural healing properties of the amniotic membrane. This is a part of the inner cavity of the placenta (lining of the womb) that nourishes a fetus in utero. It is important to know that the tissue is not a part of the fetus in any way and is harvested after the baby has been delivered through a cesarean section.
What is it?
Amnion-derived tissues come in two forms:
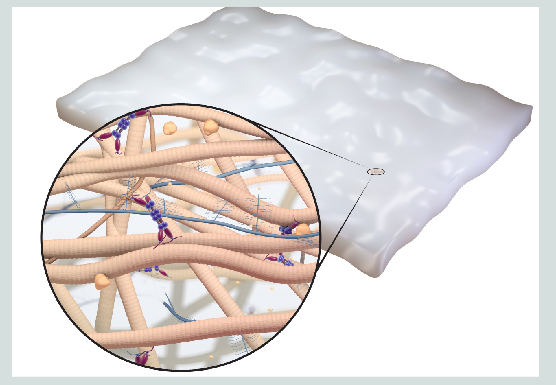
Amniotic matrix is an anatomical barrier that helps provide mechanical protection to prevent adhesion and scar formation while supporting healing with nutrient-rich growth factors.
Viscous Amnion is amniotic fluid that contains a broad spectrum of growth factors and cytokines that play an important role in wound healing, cell proliferation, tissue protection and repair. Unlike the Matrix which is a sheet of tissue used in surgery, the viscous amnio is reconstituted for injections and can be combined with PRP.
With over 100 years of clinical history, the regenerative capability of amniotic membrane is well documented. Just as amniotic tissue protects and nourishes the fetus during development, Amnio matrix helps provide the same support to damaged tissue. Viscous amnio preserves and delivers multiple extracellular matrix proteins, growth factors, cytokines and other specialty proteins. These components have been shown to activate the body’s own healing process. Due to these properties, amniotic fluid has been used in various surgical applications. Viscous amnio is used as an adjunct to another soft tissue procedure.
How is it done?
Amniotic matrix is used in surgery as an augmentation to tendon repair as with rotator cuff repair, Achilles tendon repair, or ACL repair.
Viscous amnion can be used in injections as described for PRP above. It is typically combined with another soft tissue procedure as with a tendon release for tennis elbow or as a healing adjunct after a surgical repair like those listed above.
What are the risks?
Because this tissue is harvested from another person there is always a small risk of disease transmission. All donors are screened and thoroughly tested. Otherwise, the small risk of localized pain and swelling at the site can occur but are part of the healing process.





















